The doctoral dissertation of Annika Piirainen, Lic Med, explores the dosage, administration and related adverse events of three non-steroidal anti-inflammatory drugs (NSAIDs), dexketoprofen, etoricoxib and ibuprofen, in postoperative pain management after cholecystomy, back surgery and arthroplasty.
NSAIDs are commonly used in postoperative pain management as part of multimodal analgesia. NSAIDs provide substantial analgesic efficacy after major surgery and have an opioid-sparing effect, thus reducing opioid-related adverse effects. Previously, the analgesic efficacy of NSAIDs and their risk for adverse events have been thought to be dose-dependent; therefore, finding the optimal dose is critical. Though NSAIDs are generally well-tolerated, there are concerns about their effect on perioperative bleeding and risk for acute kidney injury (AKI). These adverse events are, fortunately, rare, but their risk increases in older patients and in patients with particular co-morbidities. Major surgeries are increasingly performed on elderly, and thus, more knowledge on safe and optimal use of NSAIDs is required.
In addition, prevention of AKI by optimising perioperative treatment can improve recognition of patients at high risk for AKI as well as diagnostics of AKI. Current markers for renal insufficiency are nonspecific and confounded; there is a substantial need for more adequate biomarkers.
In the first study it was found that dexketoprofen doses of 10 mg and 50 mg provided similar analgesic effect after laparoscopic cholecystectomy. Twenty-four patients were randomised to receive 10 mg or 50 mg dose of dexketoprofen 15 minutes before the end of surgery and were given oxycodone doses every 10 minutes as rescue analgesia when clinical pain was > 3/10 at rest or >5/10 at stress until pain reduced under these limits. The minimum effective concentration (MEC) and the minimum effective analgesic concentration (MEAC) of oxycodone were recorded. There was no significant difference in total opioid consumption or MEC and MEAC of oxycodone between the two groups. Based on these results, dexketoprofen may provide sufficient analgesia with substantially lower dose than that usually advised in clinical practice.
In the second study, twenty-four patients undergoing total hip arthroplasty (THA) were randomised to receive bodyweight adjusted dose of either intravenous dexketoprofen or oral etoricoxib immediately after surgery. Plasma and cerebrospinal fluid (CSF) samples were taken up to 24 hours, and the total dose of rescue analgesia and clinical pain were recorded. Dexketoprofen and etoricoxib concentrations were analysed, as well as prostaglandin E2, interleukin 6, interleukin 10, and interleukin 1 receptor antagonist. Both etoricoxib and dexketoprofen readily penetrate into CSF; maximum concentration (Cmax) of dexketoprofen was achieved after 3 hours and Cmax of etoricoxib after 5 hours. During the first postoperative 24 hours, etoricoxib and dexketoprofen had similar effects on pro- and anti-inflammatory markers in plasma and CSF. Total opioid consumption and clinical pain were also similar between the two groups. The data imply that oral etoricoxib and intravenous dexketoprofen provide equally efficient analgesia after THA.
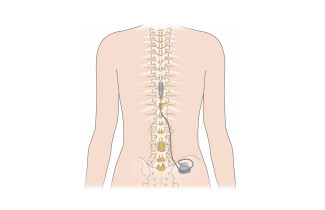
In the third study, fifteen patients undergoing back surgery were given two 200 mg orodispersible ibuprofen tablets the day before surgery and again immediately after anaesthesia and surgery. Each of the patients served as their own control. Plasma samples were taken up to six hours after administration and we compared the pharmacokinetics of ibuprofen. Anaesthesia and surgery substantially affects the pharmacokinetics of orodispersible ibuprofen; postoperative Cmax was lower compared to preoperative Cmax. However, time to maximum concentration tmax was not prolonged, therefore orodispersible ibuprofen could be used in postoperative pain management, but the dose must be optimized to ensure the analgesic concentration of 10 mg/L in plasma.
In the fourth study, the researchers evaluated the utility of novel acute kidney injury biomarkers neutrophil gelatinase associated lipocalin (NGAL), kidney injury molecule 1 (KIM-1), liver-type fatty acid binding protein (L-FABP), and interleukin 18 (IL-18) to diagnose AKI after total knee arthroplasty (TKA). Thirty patients undergoing TKA with the use of tourniquet, local infiltration analgesia and perioperative NSAIDs participated. Biomarker concentrations were analysed from plasma and urine samples that were taken preoperatively and up to 48 hours postoperatively. Only five patients had a transient decrease in urine output below 0.5 ml/kg/h reflecting mild AKI. In these patients, only plasma NGAL was increased, implying that plasma NGAL could be suitable to detect postoperative AKI.
The doctoral dissertation on Annika Piirainen, Licentiate of Medicine, entitled Non-steroidal anti-inflammatory drugs in postoperative pain management - pharmacokinetics, analgesic efficacy and renal safety, will be examined at the Faculty of Health Sciences. The Opponent in the public examination will be Professor Ilkka Pörsti of Tampere University, and the Custos will be Docent Merja Kokki of the University of Eastern Finland. The public examination will be held in Finnish on 20 August 2021 starting at 9 AM.